Many coronary heart disease patients have questions: Do I need to take medication long-term? Can I stop taking the medication once my condition stabilizes? Which medications must be taken for life?
Next, doctors from Rizhao Hospital Affiliated to Qingdao University/Rizhao International Heart Hospital will provide answers to these questions.
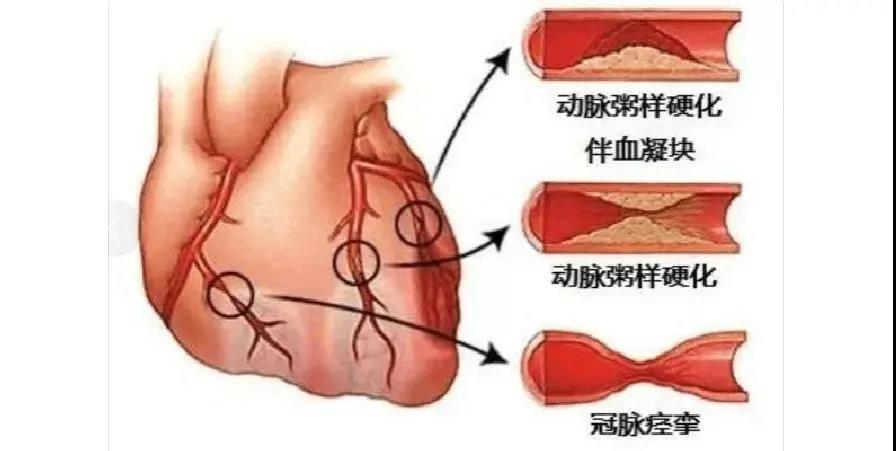
What is Coronary Heart Disease (CHD)?
Coronary heart disease refers to the narrowing or blockage of the coronary arteries due to atherosclerosis, leading to insufficient blood supply to the heart muscle, resulting in symptoms such as ischemia, hypoxia, or even heart muscle damage.
Why Do CHD Patients Need Long-Term Medication?
CHD patients are at high risk for heart attacks, strokes, and death due to severe atherosclerosis. Medications are essential for preventing these serious conditions. Therefore, long-term medication is necessary under medical advice to prevent recurrence of cardiovascular or cerebrovascular events.
Some patients may wonder, "If I have a stent, do I need lifelong medication?" In fact, long-term medication is required due to coronary heart disease, not because of the stent placement.
Which Medications Need to Be Taken Long-Term?
1. Antiplatelet Drugs
These include two main types:
1) Aspirin – A cornerstone in CHD treatment, it should be taken long-term unless there is a specific reason to stop.
2) ADP Inhibitors – Clopidogrel and ticagrelor fall into this category. After stent placement, they must be taken for at least 12 months. Most patients can stop them after a follow-up shows no issues with the stent. These drugs are critical and should never be stopped abruptly to avoid worsening the condition or serious complications.
Note:
While taking antiplatelet drugs, watch for signs of bleeding such as gum bleeding, skin bruising, or black stools. Although these medications can have side effects, they are generally safe, and patients should not stop them on their own.
2. Statins
Includes atorvastatin, rosuvastatin, and simvastatin, typically taken once at night. These drugs stabilize arterial plaque and slow or even reverse its progression, so they are recommended for long-term use in CHD patients, regardless of cholesterol levels.
Note:
Statins are generally safe but can have side effects, including liver and muscle damage. Statins may cause elevated liver enzymes, but unless the level is more than three times the upper normal limit, you can continue the medication. Liver function and creatine kinase should be monitored 4-8 weeks after starting statins and periodically every 6-12 months thereafter. If you experience fatigue, muscle weakness, or pain, see a doctor immediately, even if creatine kinase levels are normal.
3. Heart Rate Control Medications
Includes drugs like metoprolol and bisoprolol, which reduce heart rate and oxygen consumption, preventing recurrent ischemia and improving long-term outcomes for CHD patients.
Note:
Heart rate should be monitored closely while taking these medications. A resting heart rate below 50 beats per minute is not ideal. The normal resting heart rate for adults ranges between 60-100 beats per minute.
4. ACEI or ARB Drugs
Includes medications like“XXpril”or“XXsartan,”commonly used to lower blood pressure. For patients with a history of heart attack, these drugs help dilate blood vessels, improve heart function, and protect against ischemia, and therefore should be taken long-term.
Note:
The most common side effect of ACE inhibitors is a persistent dry cough. If this becomes severe, consult your doctor about switching to an ARB (angiotensin receptor blocker.
Do Not Stop Your Medications Abruptly
Coronary heart disease requires lifelong management. Even if the condition is stable, medications should only be adjusted under a doctor's guidance—never stopped on your own!
Previous article:No more
Next article:No more